Mandatory Reporting – Impairment Explained
07 Jun 2016

- a practitioner who has a blood-borne virus who practises appropriately and safely in light of their condition and complies with professional guidelines, standards and protocols would not trigger a notification
- a practitioner who has an illness which causes cognitive impairment that prevents them from practising effectively, and has no insight into their condition, would require a mandatory notification.
Problems with the mandatory reporting of impairment
Practitioners who are physically or mentally unwell may fail to seek their own treatment for fear that in doing so, they may be reported and ultimately lose their professional livelihood. These concerns may result in a delay in a practitioner seeking necessary medical care, thus increasing the risk to themselves and the patients they serve.
What changes can be made? MDA National has argued that the exception currently enjoyed by treating doctors in Western Australia should be introduced across Australia to minimise the perception (and, at times, the reality) that practitioners should be fearful of seeking treatment. Importantly, this change will bring consistency, making it a genuine National Law.
Further, the wording of the “notifiable conduct” provisions in the National Law should be amended to reflect the intended focus of the legislation on the protection of patients prospectively, rather than examining past conduct; that is, the wording should be changed to “placing the public at risk of substantial harm”, rather than “placed”.
Registration renewal: impairment question
One of the questions you are required to answer when you renew your registration by 30 September each year is:
Do you have an impairment that detrimentally affects, or is likely to detrimentally affect, your capacity to practise the profession?
If you answer “yes”, you will need to provide details of the impairment and how it is being managed. If you are unsure how to answer this question, we recommend you discuss the matter with your treating practitioner(s).
What do we know about the mandatory notification of impaired practitioners by treating doctors?
A retrospective review of mandatory notifications revealed 8% were made by treating practitioners.1 Of these, only 20% were made by the practitioner-patient’s regular care provider and 80% arose from an encounter during an acute admission, first assessment or a “corridor consultation”. The reported practitioner-patients were being treated for mental illness (44%) or substance misuse (39%).
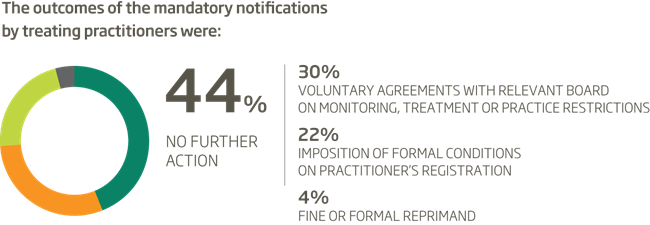
The authors of the review suggest that although almost half of the treating doctor mandatory notifications resulted in no further action, it would be erroneous to infer that these reports were inappropriate or unfounded. However, it is difficult to see how these notifications could have reached the high threshold for making a mandatory notification.
Members are encouraged to contact our Medico-legal Advisory Services team if uncertain about their obligations in a particular situation.
Dr Sara Bird
Manager, Medico-legal and Advisory Services
MDA National
See the article Mandatory Reporting of Health Practitioners for a summary of medical practitioners’ legal obligations to report another health practitioner who has behaved in a manner that constitutes notifiable conduct.
Reference
- Bismark MM, Spittal MJ, Morris JM, Studdert DM. Reporting of Health Practitioners by Their Treating Practitioner under Australia’s National Mandatory Reporting Law. Med J Aust 2016;204(1):24.e1-24.e5.
Professional boundaries in healthcare - Part 1
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding Professional Medical Indemnity Insurance
Do you understand the ins and outs of professional medical indemnity insurance?
11 Aug 2025
Professional boundaries in healthcare - Part 2
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding changes to the Fair Work Act
What are the changes to the Fair Work Act and what is my role?
22 Jul 2025