Communicating urgent pathology test results
13 Jun 2019

Pathologists who are MDA National members have had several cases where an urgent result has come in after hours and they were unable to contact the requester or their practice. They then called the patient, but the patient wouldn’t answer a call from an unknown number or the patient was suspicious about speaking to someone they didn’t know and refused to follow an instruction to go to hospital.
Such situations can lead to tragic consequences.
Real-life examples
- Delayed delivery of blood test results contributed to the death of a toddler from staphylococcus infection.1
- A cancer patient’s test results were faxed to the wrong number and media reported he died alone in a hotel room.2
- A frustrated radiologist hung up when he got the doctor’s answering service, and faxed and emailed reports of a DVT to the doctor’s surgery. The reports had not been read when the patient died from a pulmonary embolus the following day.3
The Royal College of Pathologists of Australasia (RCPA) guidelines
Guidelines from the RCPA4 include that the Requester’s responsibility does not cease with the transfer of the request to the Pathology Provider, but remains until the Requester has taken appropriate clinical action in response to the report generated by the request.
The guidelines state:
- 3.2 (1) (g) In the absence of the original Requester either during or outside normal business hours, a suitable delegate has been nominated to receive and act on the result.
- 7.1 (7) As Requesters may not always be available to receive pathology reports, they should have in place a mechanism by which Pathology Providers can communicate unexpected life-threatening test results to the Requester or their Nominated Delegate in a clinically appropriate timeframe.
- 7.2 (13) In cases where the Pathology Provider is unable to communicate life-threatening test results to the Requester or their Nominated Delegate or a suitable substitute in a clinically appropriate timeframe, the Pathology Provider should endeavour to contact the patient, or their responsible carer as appropriate.
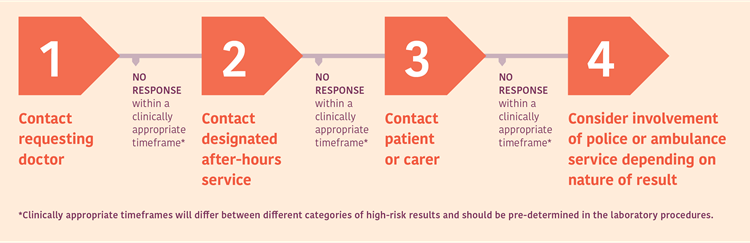
Escalation of test results
Below is an example of an escalation procedure for community patients sourced from the RCPA Guideline –Management and communication of high-risk laboratory results (jointly endorsed by RCPA and AACB).5
The Royal Australian College of General Practitioners (RACGP) guidelines
The RACGP has developed its Standards for general practices (5th edition)6 in identifying and addressing gaps in their systems.
The GP Standard 2.2E within these guidelines focuses on the follow-up of high-risk (seriously abnormal and life-threatening) results identified outside of normal opening hours, and states:
- Your practice must manage seriously abnormal and life-threatening results identified outside of normal opening hours so you can provide prompt and adequate follow-up.
- Your practice must have a process so that pathology and diagnostic services can contact the practice in urgent circumstances so information about the patient can be accessed.
- You need to explain to deputising doctors what you expect them to do if they receive urgent and life-threatening results for one of your patients, as they have a responsibility to contact the general practice in such circumstances. This could be documented in a formal agreement between your practice and the service providing after-hours care.
Ultimately, responsibility lies with both the requester and the pathology provider for keeping after-hours contact details up to date.
Karen Stephens
Risk Adviser, MDA National
Professional boundaries in healthcare - Part 1
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding Professional Medical Indemnity Insurance
Do you understand the ins and outs of professional medical indemnity insurance?
11 Aug 2025
Professional boundaries in healthcare - Part 2
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding changes to the Fair Work Act
What are the changes to the Fair Work Act and what is my role?
22 Jul 2025







