Conduct Not Notifiable
15 Mar 2017

Consider this case history. Towards the end of her rural term, an RMO found her mood was low; she was having difficulty sleeping and had lost weight.
A colleague commented that he thought her behaviour had changed and he was concerned about her wellbeing. He suggested contacting the Doctors’ Health Advisory Service (DHAS). The RMO contacted DHAS and arrangements were made for her to see a local GP. Following her consultation with the GP, a management plan was put in place to treat her depression.
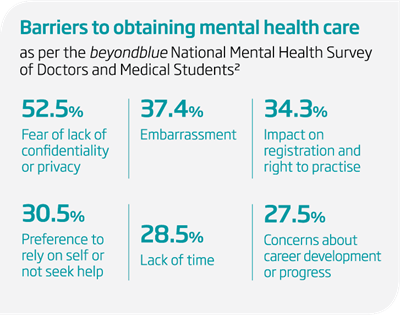
The RMO was initially reluctant to seek her own medical care as she didn’t have a GP in the area. She was concerned that seeking medical care could impact on her career and, in particular, that she may be reported to the Australian Health Practitioner Regulation Agency (AHPRA) or the Medical Board if her colleagues became aware of her depression. She was also worried that a treating GP may make a notification. This was despite the fact she had received excellent feedback from her supervisors about her progress throughout the term.
Mandatory notifications of health practitioners1
All registered health practitioners (including doctors) are required to report to AHPRA any other registered health practitioner who has behaved in a manner that constitutes “notifiable conduct”.
Notifiable conduct is defined in the National Law and means the practitioner has:
(a) practised the practitioner’s profession while intoxicated by alcohol or drugs; or
(b) engaged in sexual misconduct in connection with the practice of the practitioner’s profession; or
(c) placed the public at risk of substantial harm in the practitioner’s practice of the profession because the practitioner has an impairment; or
(d) placed the public at risk of harm because the practitioner has practised the profession in a way that constitutes a significant departure from accepted professional standards.
Impairment is defined as a person who has “a physical or mental impairment, disability, condition or disorder (including substance abuse or dependence) that detrimentally affects or is likely to detrimentally affect the person’s capacity to practise the profession”.
It’s important to note that the practitioner’s impairment must place the public at risk of substantial harm for the mandatory notification threshold to be met. In reality, this legislative requirement is no different to the longstanding ethical obligation of doctors to act if they believe a colleague’s actions are putting patients at risk of harm.
In this case, there was no risk that the RMO would be reported to AHPRA and become part of the Medical Board’s Health Program because her depression was not detrimentally impacting on her ability to work. Indeed, once she was receiving appropriate treatment, any potential risk would be substantially reduced.
All doctors must be able to access confidential care
It's important that the mandatory notification requirements involving “notifiable conduct” are not seen as an additional barrier to doctors obtaining their own health care. Of note, in WA, doctors providing health services to other health practitioners are exempt from the mandatory notification requirements.
Many doctors in specialist training have difficulty seeing their GP because they have moved or are working long hours – or they may not even have their own GP.
Every state and territory has a Doctors’ Health Advisory Service offering free 24-hour professional help to doctors and their families. It is a confidential service which can be used anonymously.
Australian Capital Territory: (02) 9437 6552
New South Wales: (02) 9437 6552
Northern Territory: (08) 8366 0250
Queensland: (07) 3833 4352
South Australia: (08) 8366 0250
Tasmania: (03) 9495 6011
Victoria: (03) 9495 6011
Western Australia: (08) 9321 3098
Dr Sara Bird
Manager, Medico-legal and Advisory Services
MDA National
References
- Australian Health Practitioner Regulation Agency. Guidelines for Mandatory Notifications. March 2014. Available at: medicalboard.gov.au/Codes-Guidelines-Policies/Guidelines-for-mandatory-notifications.aspx
- beyondblue National Mental Health Survey of Doctors and Medical Students. October 2013. Available at: beyondblue.org.au/docs/default-source/research-project-files/bl1132-report---nmhdmss-full-report_web
Professional boundaries in healthcare - Part 1
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding Professional Medical Indemnity Insurance
Do you understand the ins and outs of professional medical indemnity insurance?
11 Aug 2025
Professional boundaries in healthcare - Part 2
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding changes to the Fair Work Act
What are the changes to the Fair Work Act and what is my role?
22 Jul 2025







