New Medical Board Guidelines for Cosmetic Procedures
02 Nov 2016
What procedures do the guidelines apply to?
Under the guidelines, cosmetic medical and surgical procedures are:
“operations and other procedures that revise or change the appearance, colour, texture, structure or position of normal bodily features with the dominant purpose of achieving what the patient perceives to be a more desirable appearance or boosting the patient’s self-esteem”.
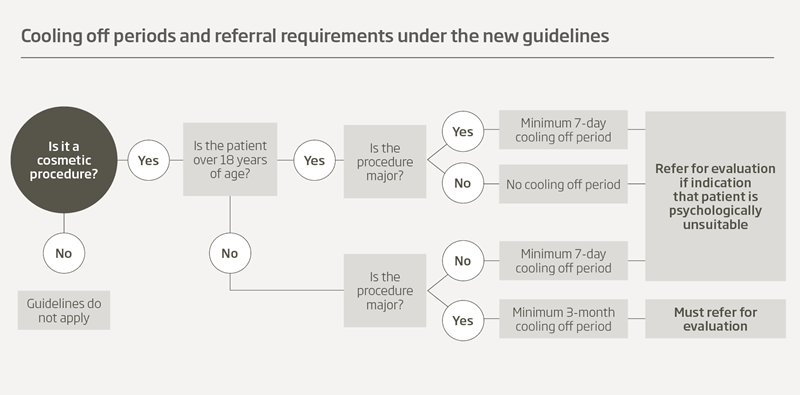
There are different requirements in the guidelines for major and minor procedures:
- Major procedures are defined as procedures which “involve cutting beneath the skin”.
Examples include: breast augmentation, breast reduction, rhinoplasty, surgical face lifts and liposuction. - Minor procedures do not involve “cutting beneath the skin, but may involve piercing the skin”.
Examples include: non-surgical varicose vein treatment, laser skin treatments, use of CO2 lasers to cut the skin, mole removal for the purposes of appearance, laser hair removal, dermabrasion, chemical peels, injections, microsclerotherapy and hair replacement therapy.
Requirements for patients under the age of 18
Medical practitioners must assess and be satisfied of the patient’s capacity to consent and, to the extent that is practicable, have regard to the views of a parent and whether they support the procedure.
The guidelines impose a mandatory cooling off period of at least:
- three months for major procedures
- seven days for minor procedures.
Further, before any major procedure, all patients must be referred for evaluation to a Psychologist, Psychiatrist or General Practitioner who works independently of the medical practitioner to evaluate any underlying psychological problems which may make them an unsuitable candidate for the procedure.
During the cooling off period, the patient should be encouraged to discuss their reasons for wanting the procedure with their General Practitioner.
Requirements for adult patients
Other than for minor procedures, there should be a cooling off period of at least seven days, the duration of which should take into consideration the nature of the procedure and the associated risks.
If there are indications that a patient has significant underlying psychological problems which may make them an unsuitable candidate for the procedure, they should be referred for evaluation to a Psychologist, Psychiatrist or General Practitioner who works independently of the medical practitioner.
Schedule 4 (prescription only) cosmetic injectables
Schedule 4 (prescription only) cosmetic injectables must not be prescribed by a medical practitioner unless they have consulted with the patient, either in person or by video. The prescribing practitioner must be contactable and able to respond if not administering the injection themselves.
Patient management and facilities
The guidelines make clear that the medical practitioner must ensure there are adequate staff, facilities and equipment, including for emergency care and treatment, during and after a procedure. Adequate written information must be given to patients on discharge, including the medical practitioner’s contact details.
Financial arrangements
Written information should be provided to patients, including the total cost of the procedure as well as possible further costs for revision surgery. Patients should be advised that most cosmetic procedures are not covered by Medicare. No deposit should be payable until after the cooling off period and the medical practitioner should not offer financing schemes.
Conclusion
The guidelines impose significant new obligations, particularly in relation to cooling off periods and for patients under the age of 18. Medical practitioners who perform cosmetic procedures are advised to review and be aware of their obligations under the guidelines.
Karen McMahon
Medico-legal Adviser (Solicitor)
MDA National
References
- Medical Board of Australia. Guidelines on Cosmetic Medical and Surgical Procedures. Available at: medicalboard.gov.au/News/2016-05-09-media-statement.aspx
Professional boundaries in healthcare - Part 1
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding Professional Medical Indemnity Insurance
Do you understand the ins and outs of professional medical indemnity insurance?
11 Aug 2025
Professional boundaries in healthcare - Part 2
Boundaries with patients present in numerous ways every day and all health practitioners
11 Aug 2025
Understanding changes to the Fair Work Act
What are the changes to the Fair Work Act and what is my role?
22 Jul 2025





